By submitting this form, you are consenting to disclose any information provided, including your name, email address, telephone number, and any other information (collectively “Personal Information”) to CSL Behring and its representatives, agents, and contractors, including CSL Behring’s support program(s) (collectively “CSL Behring Entities”) and to receive communications with relevant information from CSL Behring Entities. You may be contacted by mail, email, telephone, and/or SMS/text message in relation to our business, products, services, and educational programs intended to benefit patients using or eligible to use CSL Behring therapies. You will have the ability to opt-out from receiving communications from CSL Behring Entities at any time. CSL Behring and CSL Behring Entities will not sell your personal information. CSL Behring respects your privacy. For an explanation of how CSL Behring will use the information you are submitting, please view our Privacy Policy
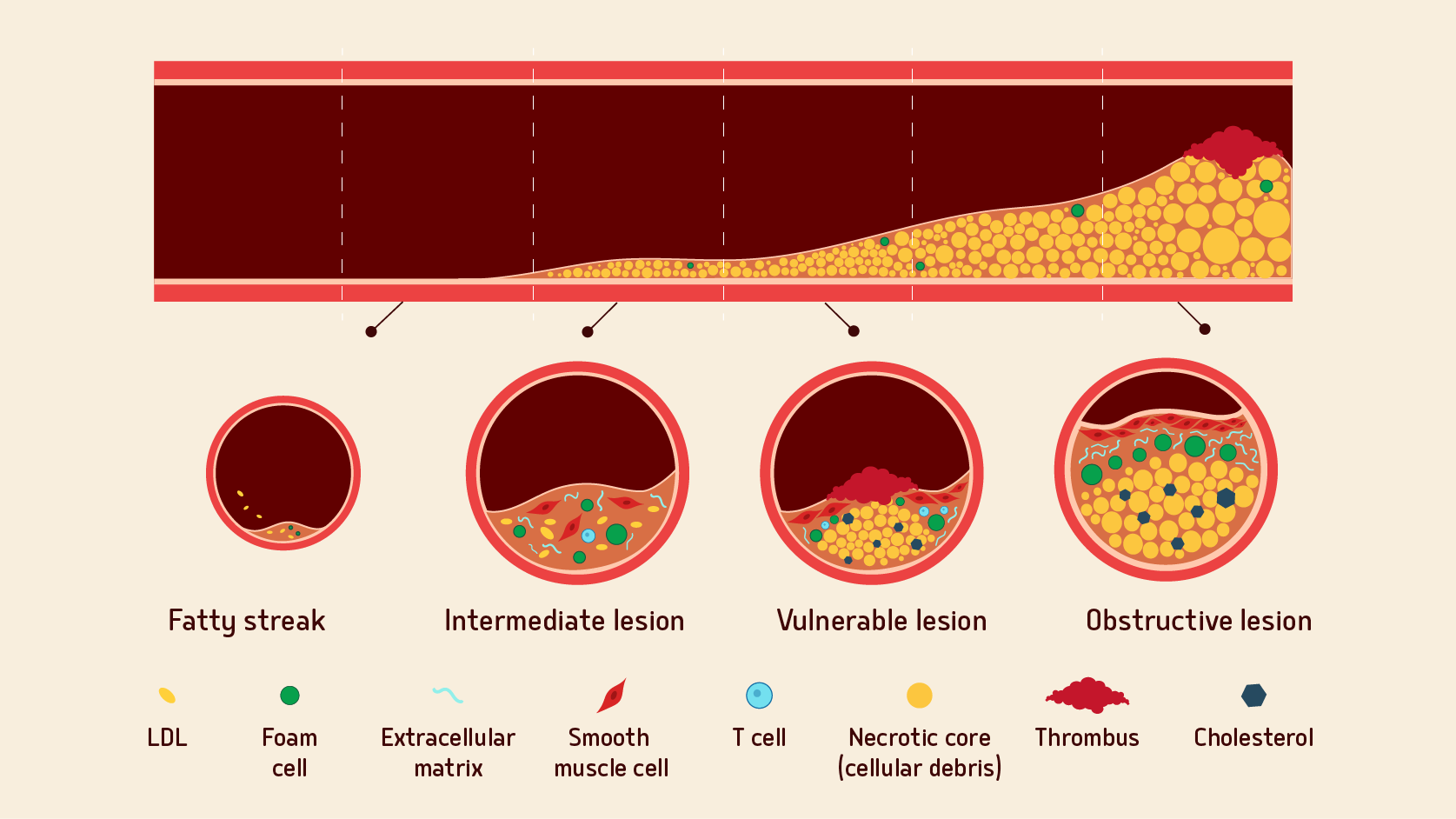
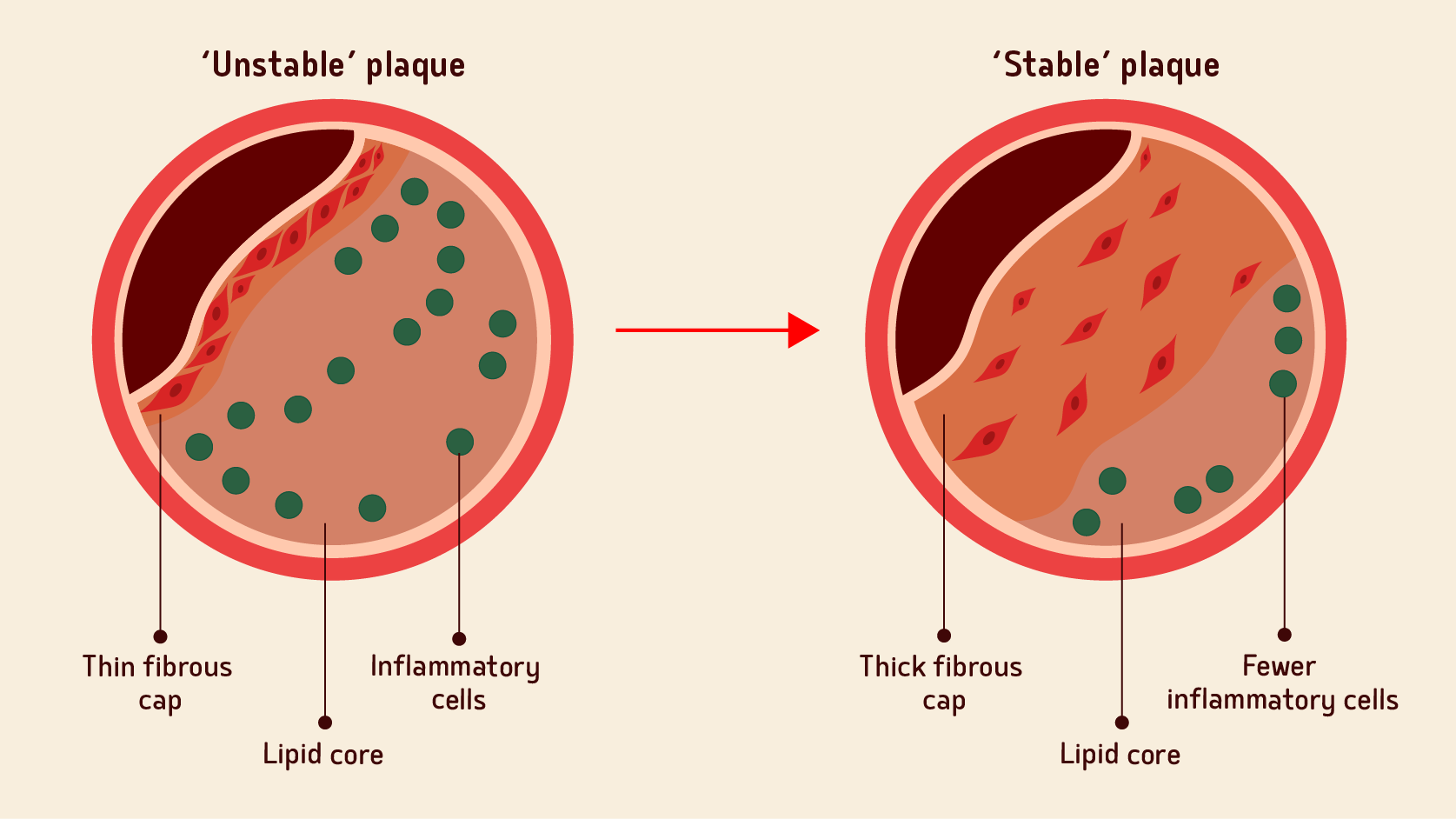
What happens to cholesterol efflux after an AMI?
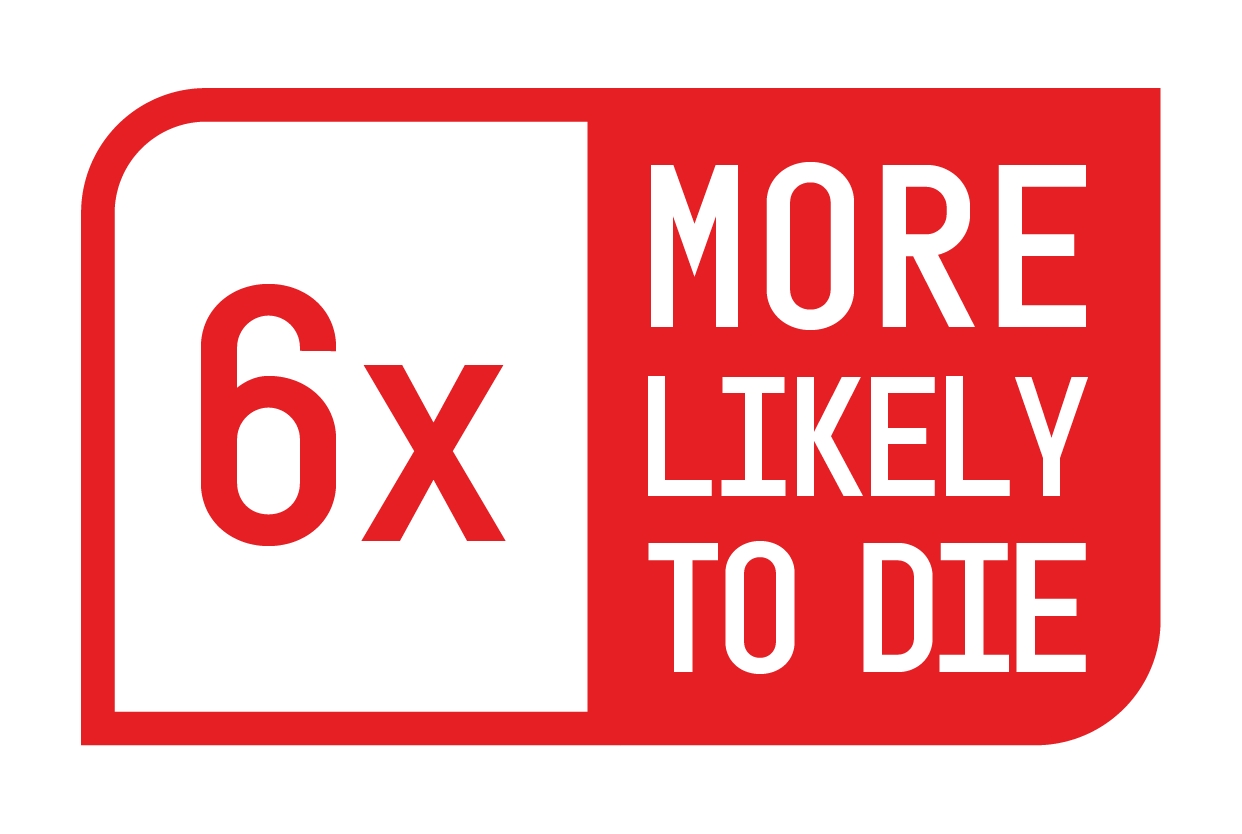
Learn about why patients are at a disproportionately high risk in the 90-day period post AMI19,20,22,25,26